Hospitals Can’t Go on Like This
Editor’s Note: The Atlantic is making vital coverage of the coronavirus available to all readers. Find the collection here.
The reports have come in from all across the country: Hospitals are filling up, especially in the Midwest, and they are running out of the staff they need to take care of patients.
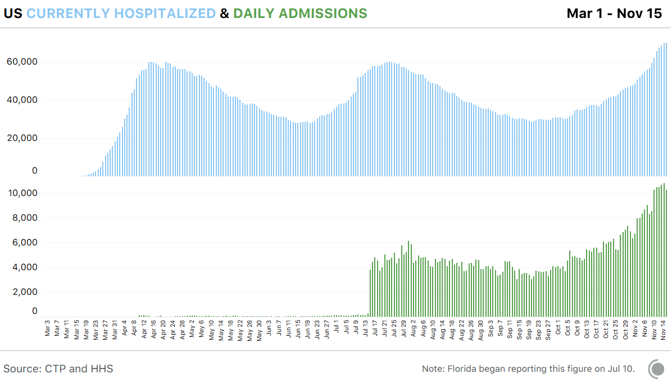
Last week, the United States broke its record from April for the number of hospitalized COVID-19 patients, blowing past 60,000 all the way to 73,000, according to data compiled by the COVID Tracking Project at The Atlantic.
Now new data released by the Department of Health and Human Services quantify the crisis in America’s hospitals in closer detail. At The Atlantic’s request, HHS provided data on the number of hospitals experiencing staffing shortages. From November 4 to November 11, 958 hospitals—19 percent of American hospitals—faced a staffing shortage. This week, 1,109 hospitals reported that they expect to face a staffing shortage. That’s 22 percent of all American hospitals.
In eight states, the situation is even more dire. More than 35 percent of hospitals in Arkansas, Missouri, North Dakota, New Mexico, Oklahoma, South Carolina, Virginia, and Wisconsin are anticipating a staffing shortage this week. COVID-19 puts pressure on hospitals in two ways. One, staff members get sick or are exposed to the coronavirus and have to stay home, reducing the labor supply. Two, more patients arrive at the hospital, increasing demand. A surge of cases makes both factors worse.
[Read: ‘No one is listening to us’]
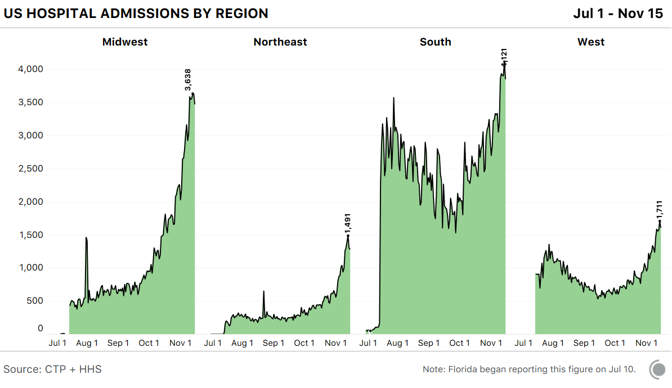
As a rule of thumb, the COVID Tracking Project has found that an increase in cases shows up as an increase in hospitalizations about 12 days later. Over the past 12 days, the seven-day average for new cases has jumped from fewer than 90,000 a day to 150,000 a day. While we’ve been able to track the number of people hospitalized with COVID-19 since March, we have not known how many new people were being admitted to hospitals each day, perhaps the best indicator of surging infections. But yesterday, HHS released this data going back to mid-July. At the peak of the summer surge, the seven-day average of daily admissions topped 5,000. Yesterday, the same measure topped 10,000. We should expect many more hospitalizations, and even worse staffing shortages, to come.
Even if a state has open hospital beds, it may not have the workers to put patients in them. “We are short of staff all times, either because they have COVID or they have some other illness, and we need to rule out COVID before we bring them back to work,” University of Wisconsin Health CEO Alan Kaplan told CNBC last week. The desperate times have led to some desperate measures. Last week, North Dakota Governor Doug Burgum ordered that health-care workers who have COVID-19 but are asymptomatic can be sent back to work. Many nurses have objected to the practice.
Even without government mandates, the shortage of workers has meant that only 36 percent of hospital nurses are “always … able to stay home when they have influenza or COVID-like symptoms,” according to a survey by National Nurses United conducted from mid-October to November 9.
[Read: The worst day of the pandemic since May]
And that was before the current surge reached its recent heights. While we don’t have data for the spring, this week’s staffing shortages have already exceeded those of the summer, according to HHS. Nearly every state in every region is showing major increases in hospital admissions. But the Midwest is up roughly seven times from its September low. That’s a lot of pressure to exert on a region’s health-care systems, especially the staff. Beds can be built, floors can be repurposed, but you can’t simply train a new legion of nurses and doctors. During past surges, which were more localized, workers could be brought in from other places, but given that the current onslaught is national, that’s going to be much more difficult.
The core issue is the same one that doctors laid out in the spring: If infections are not brought under control, too many people will end up in beleaguered hospitals, and the standard of care will fall. We largely prevented that over the summer. And measured from the spring into the summer, death rates fell. While it is not clear that this drop continued into the fall, what does seem likely is that if a region’s health-care system begins to collapse under a staffing shortage, the case-fatality rate will rise again. That is to say, unless hospitalization trends change, more people will die, and die within sight of a vaccine.
“If we can get patients into staffed beds, I feel like they’re doing better,” Eli Perencevich, an infectious-disease doctor at the University of Iowa, told my colleague Ed Yong. “But that requires a functional health-care system, and we’re at the point where we aren’t going to have that.”